Just over a week ago, my life changed for the foreseeable future. I say “foreseeable” because what’s happened is currently reversible. Though, that all depends on how my body reacts to the changes, and whether it’ll be made permanent in the future. I am stepping into the unknown, and taking it moment by moment.
You see, for the past few years I’ve been under the colorectal team at St Thomas’ Hospital in London. I’ve had many invasive tests, where all my modesty has been thrown out the window. I’ve seen myself poop via a barium X-ray study, I’ve had a balloon inserted up the bum and countless other medical devices shoved in places you’d rather keep to yourself. It’s raw writing this so openly, but the reality is up to 6.5 million of British people of all ages will have been affected by some kind of gastrointestinal disorder (Bladder and Bowel, 2023). And for many their GI disorder leads to chronic pain and complications. Yet, we still struggle with the taboo about poo!
I was diagnosed with GI dysmotility called Slow Transit Constipation. Alongside this, I’d been diagnosed with Intussusception. A condition where the bowel basically ‘telescopes’ in on itself, which can cause blockage and reduce blood flow to that part of the bowel. The way I had intussusception described to me was to ‘imagine wearing a long sleeved top, and then putting on a coat. The long sleeves begin to fold into itself, and it is really uncomfortable, that you need to try and adjust the sleeves and flatten it all out’. We’ve all been there, trying to adjust multiple layers of clothing, so imagine your bowel trying to adjust without any assistance. It doesn’t really work.
So, what do they do? Aside from the invasive tests, they might try you on various diets, and try medication which can help stimulate the gut and get it moving again. Unfortunately, this doesn’t always work and the next option may be the surgical route.
That’s the point where I’m at. I’ve spent the past 11 days at St Thomas’ Hospital following a loop ileostomy procedure. This procedure requires the surgeons to cut through the abdomen and bring a part of the bowel up to the surface, creating a ‘stoma’. With a loop ileostomy, there are two stoma parts. One which is active and leads to the small bowel. This is where there is output from the bowel into the stoma bag. The other stoma is inactive and leads to the large intestine, and can lead to some mucus bowel movement, which is totally normal. Whilst a loop ileostomy is often temporary, many people choose to keep their stoma as it increases their quality of life.
This is why I opted for the stoma.
So, what caused the issues? Of course, there are many reasons why individuals have problems with their GI system. Mostly, it is through poor diet and lack of exercise. However, for others, they may experience chronic pain, crohns or colitis, IBD or IBS, or trauma to the bowel such as cancer or injury. For some, like myself, the GI issues come with Hypermobile Spectrum Disorder (HSD)/Ehlers-Danlos Syndrome (EDS). I also have Fibromyalgia which also doesn’t help with pain levels. Then, to make things worse for myself, a history of disordered eating and laxative abuse only slowed down the bowels even more.
I tried so many things to get my gut working like the ‘normal’ average Joe, but whatever I tried, continued to increase my bathroom anxiety. I’m either going too much or not at all, and that is extremely embarrassing when you have a queue as long a double-decker bus waiting for the cubicle to free-up. I’d also got to the point where pins and needles were so severe, cutting off the blood supply, I would fall off the toilet as I tried to stand up. Again, the humiliation has been too much and I needed to find some kind of relief.
That’s where the stoma operation comes in. Yes, it’s a last resort. It’s worth trying it, but it can lead to its own set of complications. One of them being that the gut can work fine to start with, and then slow down over time and cause the same issues as before. If that occurs, they can either reverse the loop (as it won’t make any difference), or there’s a possibility of needing to be tube-fed (for the rest of your life) which is certainly beyond ideal.
Preparing for stoma surgery has taken months. I joined support groups to ask all the questions which my mind kindly gifted me as I anxiously prepped myself for what was to come. Fortunately, the ostomates had been more than helpful, sharing their experiences and their recommendations and advice enabled me to build a big picture of what life with a bag looks like.
My surgery date was moved because of the doctors strikes. This, I had found frustrating. I had mentally been building myself up for the surgery, and with days to go, my brain went into overdrive. I couldn’t keep up with it all, and I had no idea whether I was coming or going. I understood it couldn’t be helped, but it really had caused some kind of mental relapse.
A week before my surgery, I met with my stoma nurse. She visited me at home, and ‘site-marked’ me. This is where they work out the best place for the stoma to be positioned on the abdomen. It was the first time I had properly seen a stoma bag, too. Sure, I’d seen what they look like. But to have one to hand, to play around with was odd. I felt a little detached from it, with some kind of hesitation at the back of my mind. I suppose, I just wanted to get it done, so that I had no choice but to manage the bag. Playing around with one wasn’t going to teach me anything, but one attached to my body would do.
On the way up to St Thomas’, I didn’t feel any anxiety. I felt fairly calm and content, with a slight excitement that I would one day have no issues with going to the bathroom. I shouldn’t have been getting my hopes up, especially when there’s so many unknown scenarios. It wasn’t until I was in the operating theatre that the nerves kicked in. Fortunately, I was fast asleep in no time and had little time to think about pulling out. When I awoke, I ended up calling Lauren, who’d been patiently waiting for me to come out of surgery. She followed us upstairs to the ward, where I would find myself staying on for 10 days.
I thought I’d be out within 3-4 days. But, I developed a complication from the surgery – ILEUS. Ileus is when there is a blockage somewhere in the gut, often due to the trauma of the surgery. Because of this, I was extremely sick and ended up with a nasogastric tube. This tube went up my nose and into my stomach and is used to decompress the stomach. They’d use a syringe to aspirate the tube and bring out contents of the stomach so that I wasn’t sick. However, it turned out that the tube created more nausea, and was removed after 24 hours. Thank goodness, because it was awful!
Not only did I end up very sick after surgery, my mental health just plummeted. Hysterical crying only made the situation worse. I would get myself into such a state. I would stare at my tearful, red faced reflection, looking at the scar attached to my belly button, feeling grossed out by the stoma bag, and just threw a tonne of hurtful comments to myself. If ever there was a time to kick myself down (which is never btw), this was not it. I was already feeling beaten and torn.
So, what did I do? Aside from reaching out, and explaining what was going on, I looked to breathing exercises, listening to the Sleep Zone Podcast on Spotify to calm me down, and repeated positive affirmations and kind words to myself. Enough was enough. I needed to be gentle and kind. I’d been through a life-changing major operation, so it was natural to be sensitive and tearful to change. It was strange practicing this sort of self-care. But, it was something I needed to do. I tried to hone in on the ‘practice what I preach’ factor, and think back to what I would tell my clients going through their own crisis. I found myself self-coaching and ultimately grounding myself into a state of calm.
I’ve been lucky. I’ve had some ups and downs on the ward, and there’s been patients come and go. There’s only one who’s been with me since shortly after the beginning. She’d been through quite some surgery, which also involved creating a different type of stoma, called a colostomy (which uses the large bowel). And, knowing we were going through something similar, particularly with adjusting to the change of living with a stoma, we bounced off each other’s strengths. The determination for us to get home suddenly saw us bounce up a notch. Watching the recovery from being bed-bound to walking round the block (aka the ward) several times, brought great energy back into the room.
I’d also had the company of my Mum through a visit on my first full day, plus FaceTime conversations aplenty. Lots of Telegram messages being sent back and forth to Lauren, who’d been stuck in the worst shift pattern on the calendar, and daily wishes from my Dad. I’d also heard from my best friend, my sister and my work colleague. But with low energy, and my first 7-8 days being wiped out, I wasn’t able to speak to anyone. I just needed to heal.
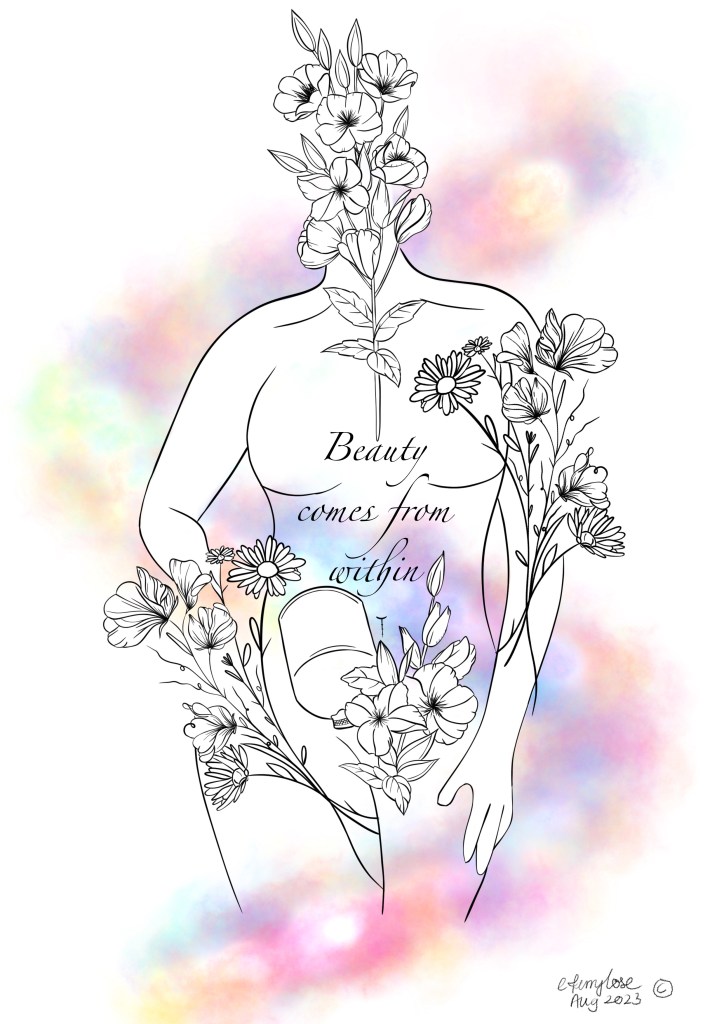
Typically, I’d taken so much with me to do in hospital, from colouring in to word searches, reading to drawing. I took my Switch (which stayed in my bag) and took along my iPad for the hope of a Marvel binge on Disney+. That, too, didn’t happen. When I felt able to, I drew up a picture on my iPad, just to allow myself to focus on what I’ve been through in a positive way. I shared it with the room, and on the stoma support group. I seem to have hit a chord. It definitely represents what we have been through, and most importantly reminds us that ‘Beauty comes from within’ (image at end of post).
I couldn’t wait to get moving. Mum had taken me downstairs in the wheelchair and we stocked up on snacks. However, these barely got touched for the first week. Then, Lauren surprised me with a visit with some of the things I’d mentioned to her that I was lacking. On this visit, she helped me shower and get dressed, plaited my hair and helped walk to the lift which would take us 11 floors below to the ground floor. We enjoyed a Costa for lunch, and as we went to head outside for some fresh air, we spotted her Aunty in the foyer, waiting for her friend, who’d both popped by to say hello! Lauren’s aunty had been up for her own hospital appointment, so it was kind of them to make the trek over to St Thomas’ to see how I was doing!
I wanted to get home. It was hard enough saying goodbye in person, or not wanting to hang up the phone. My nausea was subsiding, and there was only one last thing to tackle…
As soon as I had the opportunity to change the bag, I went for it. I couldn’t do it to start with because being in ileus meant I was so nauseous I couldn’t bear the smell, let alone the way the stoma looks. I’d been working really hard to get moving and I knew it was down to the stoma nurse to sign me off from some stoma education. Only then, could I go home!
I had an allergic reaction to the adhesive of the barrier we were using. So the stoma nurse switched brands and got me on an antihistamine. I’d developed a rash and blisters, so it was really itchy. The last thing I needed was a fresh allergy wound to be covered by another barrier, thus not allowing the skin to heal. Problem is, I had no choice. The barrier, known as a ‘flange’, is used to protect the skin around the stoma. Then the bag sits over the stoma and fixes itself to the flange and the rest of the bag has a massive adhesive loop which sticks itself to the surface of my abdomen. Fortunately, no reactions to the bag (so far!)
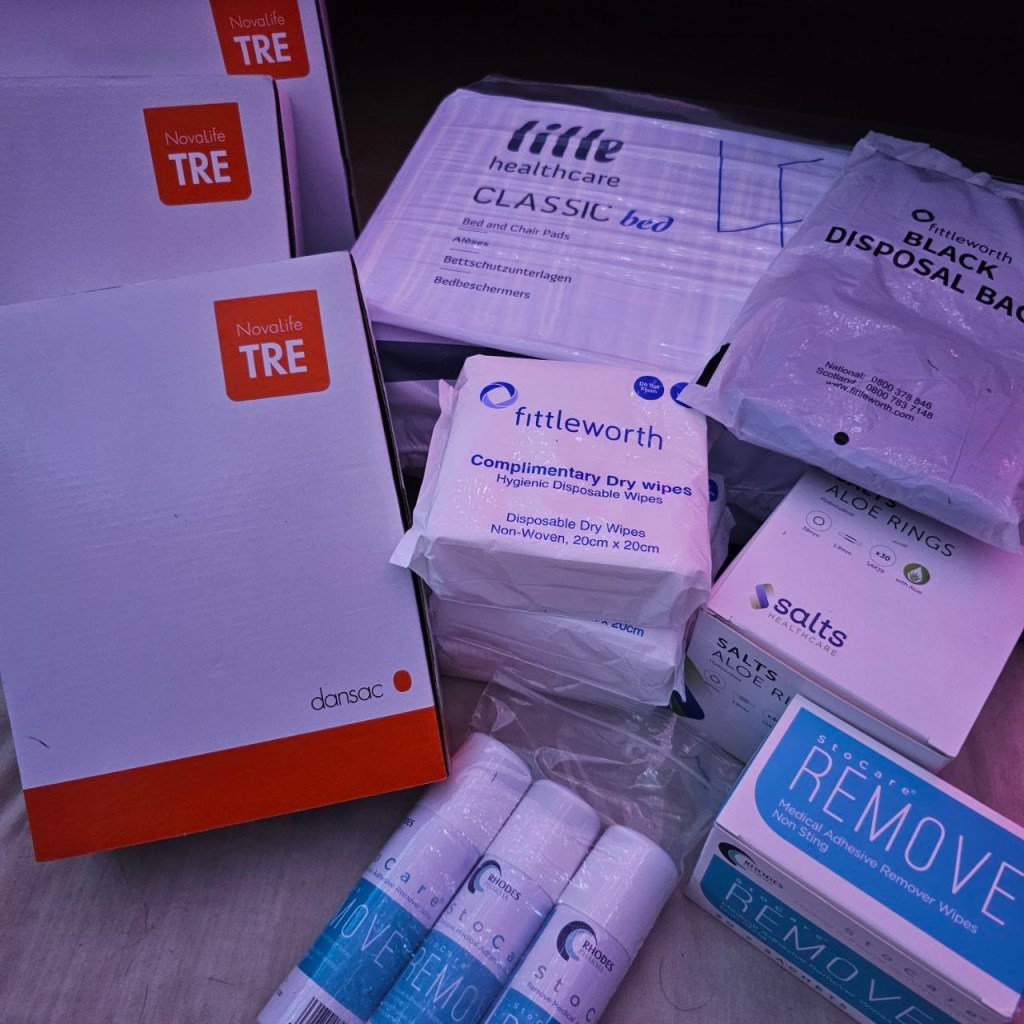
Once I’d been able to change the bag a couple of times by myself, the stoma nurse said from a technical point of view, he didn’t see why I couldn’t go home! So, he organised a lovely pack of supplies for me to take home, and explained I’d have a delivery of supplies as well to keep me going, until my local stoma nurse can help me with setting up repeat prescriptions.

I was so excited to get home. But at the same time, it felt odd leaving the room I’d spent 10 days of my life in. It was sad to sad goodbye to my fellow ostomate, as we’d been supporting each other post-op. But I knew her discharge date wasn’t too far behind me. We plan on keeping in touch and continuing the recovery journey together.
When I left the hospital, I felt like I’d absconded. It was such an odd feeling. The journey home was painful. Each road bump added to the pain I have been feeling since the op. But when I got home, being able to see my furbabies and relax, made me realise I would most definitely recover better here.
So, here we are. This is it. My new lease of life.
And as some people name their stoma to break the taboo of being able to talk about all things ‘poo’. So, I am introducing mine to you…
Meet Tommy.
And finally, in the words of Tim Minchin:
“This is my body
And I live in it
It’s 31
And 6 months old
It’s changed a lot since it was new
It’s done stuff it wasn’t built to do
I often try to fill it up with wine
And the weirdest thing about it is
I spend so much time hating it
But it never says a bad word about me
This is my body
And it’s fine
It’s where I spend the vast majority of my time
It’s not perfect
But it’s mine
It’s not perfect”
